What is a vitrectomy?
A vitrectomy is a highly specialised surgical procedure where the vitreous humour is removed from the eye. The vitreous humour fills the back four-fifths of the eyeball; the space behind the lens. There are various reasons why you might need a vitrectomy. The ophthalmologist who examines you will inform you that you might require a vitrectomy and then refer you to an eye specialist that performs these procedures.

Figure 1
Due to improved instrumentation over the last 20 years (figure 1) this procedure is currently done through tiny trocars (usually 3) placed in the side of the eye, 3.5mm – 4mm from the edge where the colour part of your eye stops and the white part starts (figure 2).
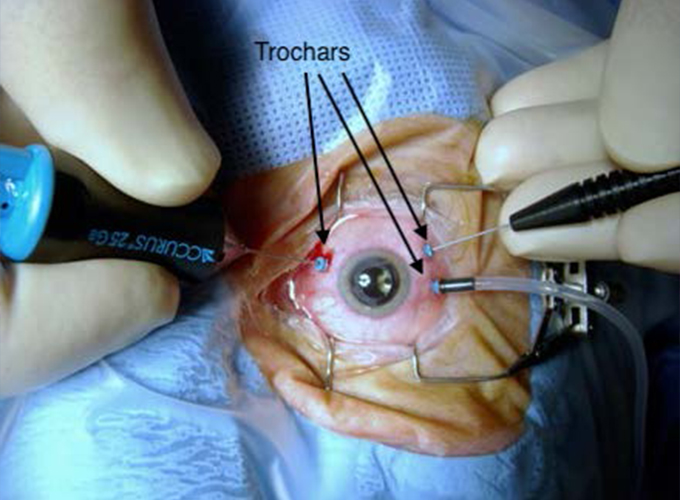
Figure 2
This is a painless procedure performed in theatre, either under general anaesthesia or local anaesthesia. Dr Enslin Uys performs 80-90% of his cases under local anaesthesia with sedation. This helps with a much quicker recovery after surgery, no sore throat from a tube that was placed down your throat and minimal side effects from anaesthetic drugs. The vitreous is removed from the eye to treat various retinal problems.
Some of the common conditions that will be discussed include the following:
- Retinal detachment
- Vitreous haemorrhage
- Diabetic eye disease
- Macular hole repair
- Epiretinal membrane removal
Retinal detachment:
Patients usually present with a new onset of floaters, a new onset of flashing lights and a dark shadow in the peripheral vision that does not go away. This may be described as a curtain over part of the field of vision. In about 7% of cases both eyes are affected. The symptoms are painless.
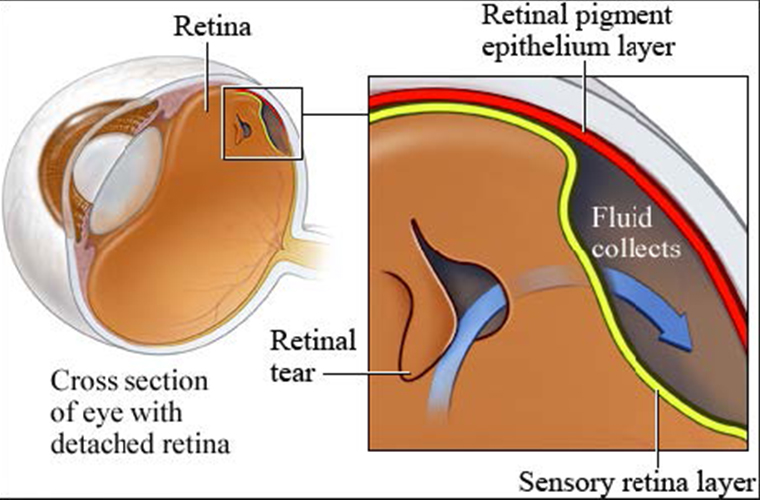
Figure 3
A retinal detachment happens after a tear develops in the retina and fluid passes through the tear (figure 3) ending behind the retina and therefore separating the retina from the underlying layer (retinal pigment epithelium). This is referred to as a rhegmatogenous (rhegma = tear) retinal detachment (figure 4).

Figure 4
Risk factors to develop a retinal detachment include the following: severe myopia (near sighted), retinal tears, ocular trauma, and a family history of retinal detachments as well as complications from cataract surgery. Without treatment, permanent loss of vision may occur. Currently 80-90 % of retinal detachments are repaired by performing a vitrectomy. This is performed in theatre, the vitreous traction is removed and a laser is applied around the tear (figure 5) to create a strong adhesion to prevent a similar episode. In most cases a gas bubble or silicone oil bubble is inserted into the eye. The gas bubble or silicone oil helps to close the tear by pushing the retina and surrounding tissue together while the laser burns around the tear, forming an adhesion between the layers which strengthens over 7-10 days. The gas bubble gets smaller over time and eventually disappears, as opposed to the silicone oil bubble that has to be removed later with another operation. Gas inside the eye and the difference in altitude between various places (even flying) plays an important role that Dr Enslin Uys will discuss with you.

Figure 5
Retinal detachments can also be repaired from the outside (10-20%) by placing a silicone tyre or buckle over the break, followed by applying a laser or cryo (freezing) around the tear to create a strong adhesion and prevent a similar problem. In 90-95% of cases one surgical procedure will be enough to sort out the problem; unfortunately 5-10% of patients will need more than one surgery.
Vitreous haemorrhage:
There are a number of reasons for a vitreous haemorrhage which include the following: retinal tear, retinal detachment, abnormal new vessel formation secondary to diabetes, vein occlusions, following ocular trauma, macro aneurysm or even wet age related macular degeneration. In order for the ophthalmologist to see the back of the eye and determine the cause for the bleed, the blood needs to be removed by doing a vitrectomy (figure 6). An ultrasound can be performed through the blood to make sure the retina is not detached, but the exact cause cannot always be determined with an ultrasound.
Diabetic eye disease:
The most common reasons for doing a vitrectomy, in a diabetic patient, are due to vitreous haemorrhage, tractional retinal detachment, epiretinal membrane formation and progression of diabetic eye disease despite adequate argon laser therapy. A tractional retinal detachment differs from a rhegmatogenous retinal detachment, as there is no hole in the retina.
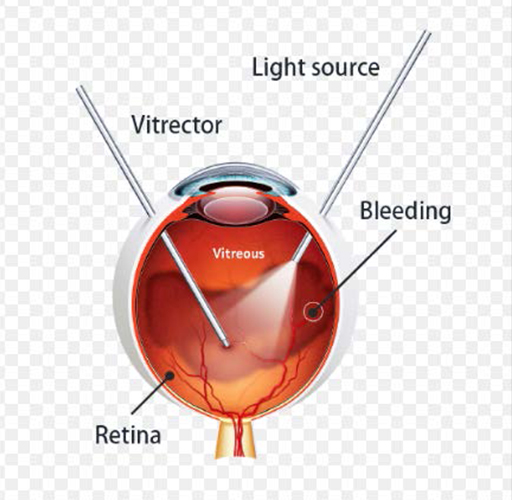
Figure 6
or followed by an eye injury. Regular routine eye examinations are very important for all patients with diabetes to treat early diabetic eye disease and prevent blindness.
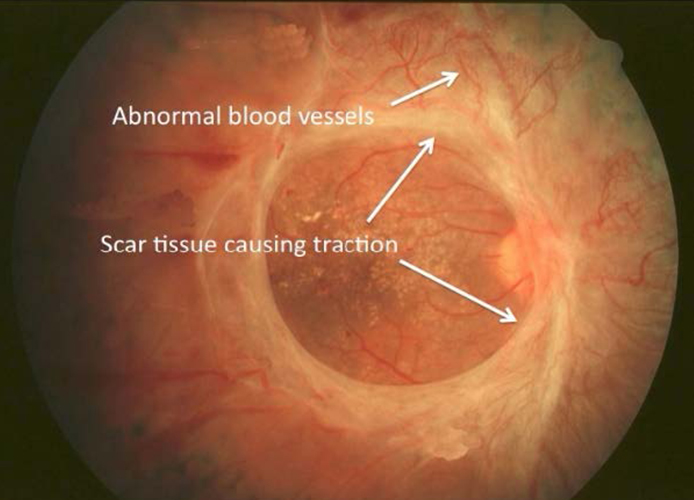
Figure 7
Macular hole:
A macular hole refers to a small tear or hole in the centre of the macula area (fovea) of the eye (figure 8). Because the centre of the macula is essential for clear and detailed vision needed for tasks such as reading and driving, a 4 hole in this area (figure 9) causes distorted vision or a dark patch in the centre of your vision. If a macular hole develops in one eye, there is a 5% to 15% risk of one developing in the other eye.
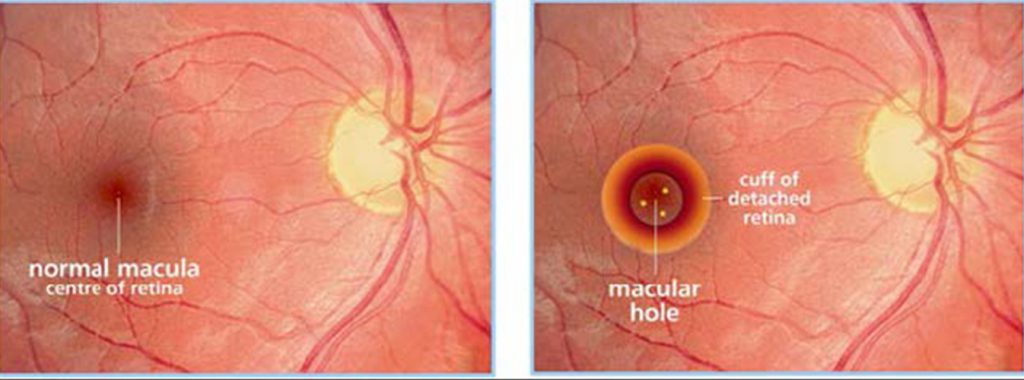
Figure 8 & 9
Optical coherence tomography (OCT) is the current gold standard in the diagnosis (figure 10), staging, and management of macular holes. This quick, non-invasive imaging technique allows for evaluation of the macula in high resolution using reflected light, and helps your doctor differentiate a hole from other eye conditions with similar symptoms.
Rarely, very early macular holes repair themselves. In most cases macular hole surgery is required to repair the tissue and improve vision. Vision loss is slow, painless and progressive, often starting only as distortion of one’s central vision. The best visual results are obtained when these holes are closed early (< 6 months duration) and when they are small. During the procedure, Dr Enslin Uys will first remove the vitreous gel by performing a vitrectomy, followed by peeling the internal limiting membrane, which is the most inner layer of the retina and thinner than newspaper. The vitreous cavity will be filled with an air bubble made from a special gas, which keeps the macular hole in a stable position as it heals. The gas bubble slowly goes away on its own over several weeks. Positioning one’s head or face down for the first 3 days is uncomfortable but very important in the healing process and success of closure of the macular hole.
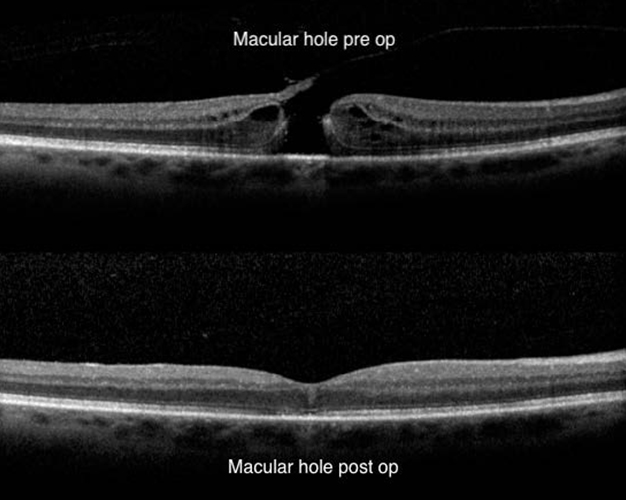
Figure 10
Epiretinal membrane removal:
An epiretinal membrane (figure 11) is a thin layer of tissue that sometimes develops on the retina over the area of best vision – called the macula. It is also sometimes called cellophane maculopathy or macular pucker. The membrane can affect someone’s vision and can occur for a number of reasons. This includes previous retinal detachment, inflammatory eye disease, or as a result of an eye injury, and can be removed surgically. During the epiretinal membrane surgery, Dr Enslin Uys will first perform a vitrectomy that is followed by gently peeling away the membrane from the retinal surface, using small surgical tools or mini forceps.

Figure 11
In summary:
Of all the conditions discussed above, the only medical emergency is a rhegmatogenous retinal detachment. If you have a new onset of floaters, a new onset of flashing lights and/or a dark shadow in your peripheral vision that does not go away contact your ophthalmologist, GP or local optometrist immediately. You will need to be seen urgently (within 24hours).
All the other conditions discussed will cause slow, progressive, painless loss of vision over a period of time that needs non-urgent referral (within a few weeks).



